Telescopic Denture From Start to Finish
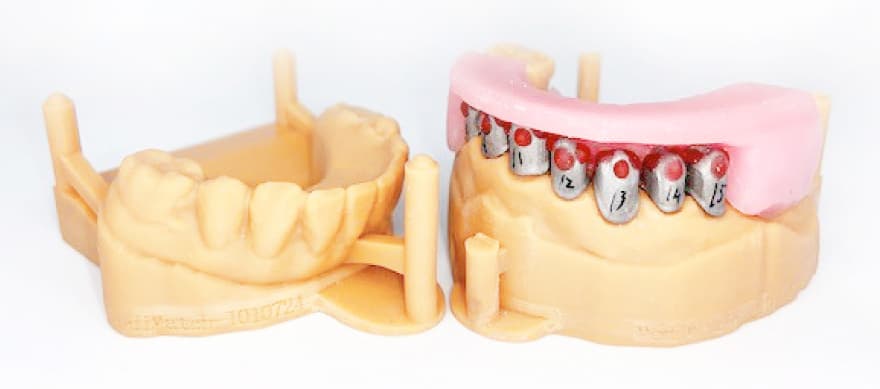
Producing a Telescopic Denture
STEP 1 – First surgery visit
- Take upper and lower full arch silicon impressions.
- Send impressions to the lab.
STEP 2 – In lab
- Cast models.
- Make upper primer (inner crowns) for telescopic denture.
- Make upper wax bite block.
- Make upper special tray with holes.
STEP 3 – Second surgery visit
- Try primer crowns in the patient mouth (inner crowns).
- DO NOT CEMENT ANYTHING AT THIS STAGE.
- Record the bite using wax bite enclosed.
- Take silicon pick up impression of the inner crowns using the special tray enclosed.
- Send the impression for the attention of lab manger to ensure impression is casted in the correct manner.


STEP 4 – In Lab
- Cast model.
- Make secondary crowns on top of the primers enclosed.
- Make upper metal frame with acrylic teeth set up in wax.
- Weld the secondary crowns to the frame. Build up the secondary crowns in composite.

STEP 5 – Third surgery visit
- Without cementing anything at this stage, try the fit of the frame with the inner crowns in the patient’s mouth.
- Ensure to check the fit and shade.
- If you need any adjustment (to the frame design) let the lab know at this stage.
- If you are pleased with the aesthetics send the work back to the lab to be finished.
- It is very important not to lose any components and not to cement anything at this stage.
STEP 6 – Final in lab
- Finish the upper frame in veined acrylic.
- Send everything back to the surgery.
STEP 7 – Final surgery visit
Ensure all crowns/primers are attached to the frame and place everything in the mouth at the same time. Cement only one or two primers at a time, repeat this process until all primers are cemented.
Indications for a telescopic denture


Patient has:
- Few remaining or unfavourably distributed abutment teeth.
- Extensive caries or poor contour on abutment teeth that therefore need to be covered by crowns.
- Advanced periodontitis.
- Abutment teeth that are not parallel, making path of insertion difficult to find.
- Oral cancer.
- Undergone occlusal reconstruction.
- Poor manual dexterity.
Advantages
Good Retention and Stabilization
The great retentive force is a result of the accurate contact and tight fit between the inner and outer crown surfaces.
Retention
Occlusal forces transferred through the long axis of abutments is achieved because the crowns surround the abutments.
Common Path of Insertion
This can be easily created as the inner crowns surround the abutment.
Easy to Keep Clean
As the denture can be removed, this allows an effective home oral hygiene regime. The excellent fit of the inner crown of the abutment may protect the tooth from caries.
Aesthetics
The double crown technique is more aesthetic than a conventional denture as there are no visible clasps.
Ease of Repair and Adjustment
Telescopic dentures can be easily repaired, even when an abutment has been lost.
Disadvantages
Length of Completion
The fabrication contains complicated clinical and laboratory procedures, which can result in the treatment period being long and increased costs.
Retentive Problems
The retention of the denture can only be evaluated after cementation of the crowns. The repeated removal and insertion of the denture will eventually decrease the retentive mechanical force as the metal wears.
Cervical Caries
If the crowns do not accurately cover the whole of the abutment and the patient has poor oral hygiene, cervical caries may occur.
Extensive Follow up Required
Technical failures may occur such as loss of cementation, loss of facings, fracture of artificial teeth, and fracture of framework or denture base. Therefore, regular appointments for assessment and maintenance is necessary to prevent failures.
Legal disclaimer
In addition to MediMatch’s normal terms and conditions we would like to point out that:
- This protocol is based on very limited experience Medimatch has with their cases and should only be used as an indication and not restrictive in any way or form.
- This protocol was not based on experience in a clinical environment. Clinicians will use their own technique, according to individual experience and training.
- This protocol should not be followed if the circumstances are different or if in any way or form it is clinically not appropriate to follow it even if the circumstances are similar as in the protocol.
Each clinician should make their own decisions and not be restricted to following a protocol made by Medimatch Dental Laboratory Ltd. - MediMatch Dental Laboratory Ltd is in no way liable for any clinical procedures and will not take responsibility for the use of the content of this protocol in a clinical or non clinical environment.
Each clinician is ultimately responsible for their own clinical decisions regardless of any advice given by MediMatch Dental Laboratory Ltd in any form.